IFCHC e-Newsletter 2021.02
News and stories from IFCHC member Community Health Centres and CHC associations around the world
Addressing social and cultural stigma related barriers to care: New research and tools from Toronto, Canada’s Access Alliance
 On Wednesday, August 4, Access Alliance Multicultural Health and Community Services (Access Alliance), an IFCHC member Community Health Centre based in Toronto, Canada, announced the release of Tackling TB Stigma: A Cross-Sectoral Approach to Reducing Tuberculosis (TB) Stigma and Improving TB Care for Vulnerable Newcomer Populations in Canada. The report was the result of comprehensive, community-driven research that sought to examine TB-related stigma and highlight recommendations for effectively addressing stigma around diseases.
On Wednesday, August 4, Access Alliance Multicultural Health and Community Services (Access Alliance), an IFCHC member Community Health Centre based in Toronto, Canada, announced the release of Tackling TB Stigma: A Cross-Sectoral Approach to Reducing Tuberculosis (TB) Stigma and Improving TB Care for Vulnerable Newcomer Populations in Canada. The report was the result of comprehensive, community-driven research that sought to examine TB-related stigma and highlight recommendations for effectively addressing stigma around diseases.
“The findings in this report are drawn from the unique experiences of newcomers to Canada, their descriptions and observations of the particular kinds of stigma they’ve faced, and their experiences of what has worked to help them address tuberculosis and other health challenges,” said Cliff Ledwos, Director of Primary Care and Associate Executive Director at Access Alliance. “Coordinated collaboration across health and social sectors that interact with newcomers, to ensure timely and sustained access to wraparound health services, is one of the big keys to ensuring that stigma and other barriers to health and wellbeing are addressed, and people can get the supports they need.”
Access Alliance has recently applied for additional funding to action recommendations from the report, including the development of a centralized intake system to support community members in connecting to the wraparound services that result in positive health outcomes and equitable care. In addition, the report demonstrates that when the research process is community-led, the information that is generated from research can provide immediate benefits. Wilma Miravalles, one of the community research participants, was a direct beneficiary of knowledge collected for the report.
Born in the Philippines, Wilma has first-hand experience of the impacts that TB stigma can have on an individual. “I have a family member that has TB and we always distanced ourselves from him—being in this study really opened my mind, and I shared the information with my family in the Philippines,” said Wilma Miravalles, Community Research Participant. “If I had this knowledge about TB I would say that I would have acted differently as it relates to TB. All this information about TB changed our mind—I had so much fun doing the study because I learned a lot.”
While the report highlights TB and its impact on newcomer populations, disease-related stigma and the factors that pose barriers to accessing comprehensive healthcare go beyond TB. Access Alliance is currently producing an issues report on reducing inequities in cervical cancer screening among newcomer women, which explores self-screening as an alternate modality to Pap tests. While the report has not yet been published, research has found that stigma surrounding the topics of sexuality and sexual health, among other factors, result in newcomer and immigrant women having a significantly higher risk of being under-screened for cervical cancer compared to Canadian-born women.
In the case of both TB and Cervical Cancer screening, community-based and culturally responsive care pathways are necessary to ensure positive health outcomes for immigrant and newcomer communities. Developing these pathways will result in systemic change, and meaningfully engaging community members in the research that is required to develop effective programs can provide immediate benefits for those individuals and their peers.
Additional products, including Fact Sheets for key stakeholders, are available in English and French on Access Alliance’s Tackling TB Stigma page.
Counselling Connect: ensuring low barrier access to prevention-focused counselling services in Ottawa, Canada
Counselling Connect (CC) is a COVID-19 born innovation and collaboration of Community Health Centres and community based mental health and addictions organizations in Ottawa, Canada, that leverages a digital platform and virtual care to connect children, families, youth, adults and older adults to prevention-oriented mental health and addictions care in three languages: French, English and Arabic. IFCHC Members Centretown Community Health Centre, Somerset West Community Health Centre and Sandy Hill Community Health Centre have played key roles.
is a COVID-19 born innovation and collaboration of Community Health Centres and community based mental health and addictions organizations in Ottawa, Canada, that leverages a digital platform and virtual care to connect children, families, youth, adults and older adults to prevention-oriented mental health and addictions care in three languages: French, English and Arabic. IFCHC Members Centretown Community Health Centre, Somerset West Community Health Centre and Sandy Hill Community Health Centre have played key roles.
Before the pandemic, people in Ottawa and surrounding regions received free counselling services mainly through community walk-in services. But with COVID-19 restrictions, in person appointments were not available. Organizations knew that mental health and addictions support needs were going to increase exponentially and that there was an urgency to ensure people had timely access to existing services. CC partners came together to pool their resources and ensure rapid, easy, and low barrier access to existing prevention focused counselling services. Counselling Connect includes:
- Easy online quick access to single-session counselling appointments – no waitlist
- Access to a skilled mental health and addictions professional from a trusted, community-based mental health and addictions organization
- Culturally welcoming services available for Francophone, Indigenous, LGBT2SQ+, and African, Caribbean and Black communities.
- A prevention model: For most, the single session is sufficient and helpful to address clients’ distress and/or concern (Hymmen and Stalker, 2013 Hoyt; Talmon, 1990)
Since its launch Counselling Connect has had a remarkable impact:
- More than 9,000 same day/next day virtual counselling sessions booked between May 2020 and July 2021
- 40% of appointments booked through partner organizations, 60% are booked by the clients themselves through the CC website.
- Clients ranging from 2 to 95 years old
- 23 partnering organizations (over 100 counsellors!) pooling resources and providing services through a single access point
- Equitable access: By the community, for the community services for individuals from Francophone, LGBT2SQ+, African, Caribbean and Black, and Indigenous communities
- Results from a snapshot client feedback survey (n=40) indicated that 97% of clients felt the counselling session they received met their needs at the time.
The Counselling Connect service model has also now been replicated in other Canadian provinces, including Alberta and Saskatchewan. CC builds connections between partnering organizations. Working through a single website and shared booking platform allows service providers to pool counselling resources, respond to community demand, and collectively coordinate service delivery.
JOIN US! Not yet a member of IFCHC? Learn how your Community Health Centre or CHC association can join and be part of the global CHC movement.
NHCW21: We wish our colleagues at the U.S. National Association of Community Health Centers (NACHC), and all state-level CHC associations and individual CHCs throughout the United States a happy U.S. National Health Center Week! Learn more and follow the hashtags #NHCW2021 and #NHCW21 on Twitter and other social media.
IN BRIEF: As regions gradually re-open, two of our state/regional CHC association members in the U.S. — Northwest Regional Primary Care Association (NWRPCA) and Community Health Association of Mountain/Plains States (CHAMPS) — are pleased to announce their joint Fall 2021 conference in Seattle, Washington, USA. The conference Re∙connect ∙ Re∙envisioning Community Health for 2022 & Beyond is accessible in person or through virtual participation.
IN BRIEF: Check out the Spring 2021 newsletter from our CHC association member, the British Columbia Association of Community Health Centres (BCACHC) headquartered in Victoria, BC, Canada.
Social Prescribing at IPC Health in Melbourne, Australia
 Based in Melbourne, IPC Health is one of the largest Community Health Centres in the state of Victoria, Australia. Through a single point of contact, IPC Health connects their clients to a full spectrum of care and support using consistent and collaborative integrated care approaches.
Based in Melbourne, IPC Health is one of the largest Community Health Centres in the state of Victoria, Australia. Through a single point of contact, IPC Health connects their clients to a full spectrum of care and support using consistent and collaborative integrated care approaches.
The CHC’s six campuses provide a diverse range of services to the community including medical, dental, allied health, psychosocial services such as general counselling, gambler’s help, and alcohol and other drugs counselling, and aged care services including home care packages.
The organization also works with local communities to address and strengthen major contributors to wellbeing and quality of living, for example in the areas of family violence, child and family services, activity groups, health promotion and community strengthening.
Beginning in July 2019, IPC Health partnered with North Western Melbourne Primary Health Network (NWPHN), Brimbank City Council, and the Australian Health Policy Collaboration at Victoria University to pilot a small scale social prescribing project, with a three stage process of research, testing and implementation at IPC Health’s Deer Park campus and within the Brimbank community. Brimbank is in the third lowest index of socio-economic disadvantage in the state of Victoria. The City of Brimbank was chosen due to the following rates of health risks:
- Second lowest participation in health enhancing physical activity
- 1 in 5 people have poor to fair self -reported health status for (38% above Australian rate)
- 10.2% of adults have mental health conditions compared to 7.9% average in Melbourne
- 1 in 8 men with high or very high psychological stress (37% above the Australian rate)
- Sixth highest rate of diabetes in greater Melbourne (63% above Australian average)
- Low learning achievement in early school leavers (15yrs) and/ or young adults with poor employment prospects: 14.2 % of youth (15-24yrs) unemployed (16% greater than Australia)
- Poor English proficiency in Brimbank that is three times that of Melbourne
 The Social Prescribing program endeavours to systematically build pathways that make use of community organisations as assets for the delivery of health and wellbeing interventions. It adopts a holistic approach using social prescriptions (social, therapeutic and practical support) to complement traditional forms of health care and move people towards prevention through factors that are protection of health and wellbeing.
The Social Prescribing program endeavours to systematically build pathways that make use of community organisations as assets for the delivery of health and wellbeing interventions. It adopts a holistic approach using social prescriptions (social, therapeutic and practical support) to complement traditional forms of health care and move people towards prevention through factors that are protection of health and wellbeing.
Similar approaches are widely implemented in the United Kingdom and Canada with expanding evidence of positive impacts on mental and physical health outcomes. While there has been less development in Australia, on 9 May 2021 the Victoria Government announced funding for Social Prescribing trials in their 2021 State Budget. Pilots will be established across eight Victorian regions and operate for three years in partnership with Victoria’s new local mental health and wellbeing services.
IPC Health is encouraged by the record amount of spending in this area and that the state government is acting on the findings of the Royal Commission into Victoria’s Mental Health System. IPC Health’s CEO Jayne Nelson said, “Working in the under-resourced growth corridor of west Melbourne, we see the impacts of long waiting lists and being unable to access appropriate levels of help before mental health issues start to escalate. As a Community Health Centre, with extensive knowledge of how social prescribing can be implemented within the Australian service system context, we are well placed to have greater impact on our diverse communities.”
By introducing social prescribing for individuals for whom traditional forms of medical/health care alone are insufficient, IPC’s pilot project is helping demonstrate that this approach can:
- improve the psychosocial wellbeing of Social Prescribing clients
- reduce the burden of workload for clinicians
- prevent escalation of potentially complex health risks and avoidable emergency department presentations
IPC’s project model is delivered by a multidisciplinary team including nurses, social workers, and counsellors who function as Wellbeing Coordinators. This integrated approach allows the client to receive evidence-based support from a range of health care professionals in a community setting. It also brings together a diverse collective of backgrounds which results in rich peer-to-peer learning experiences and opportunities for reflective practice.
The COVID-19 pandemic significantly impacted the delivery of the pilot as multiple hard lockdowns forced the closure of community centres and non-essential services, pushing planned activity and social groups online. This, in turn, resulted in limited options for fulfilling social prescriptions. Despite this, IPC Health received 477 referrals from June 2019 to July 2021.
Having established a feasible model of care for social prescribing in Brimbank, IPC Health was pleased to receive further funding from the NWMPHN in December 2020, extending the collaborative into the neighbouring Local Government Area of Wyndham. Together IPC Health and NWMPHN aim to collect patient reported health outcome measures and patient reported experience measures to improve the current knowledge base for social prescribing benefits within an Australian context. IPC Health looks forward to sharing more insights over the months ahead.
Follow IPC Health’s social prescribing journey via their website. Connect with IPC Health on Facebook, Twitter and LinkedIn.
Patricia’s* Social Prescribing story
*Name and identifying features have been changed.
Patricia is a woman in her 70s from the western suburbs of Melbourne. She lives independently and doesn’t have any in home supports. Her adult daughter and grandchildren used to visit her, however, they recently moved away from Melbourne. This meant Patricia lost her regular social interaction.
At her appointment with her IPC Health general practitioner (GP), she mentioned that she was feeling lonely and missing her family. Without her family around, Patricia was less active and she noticed that she wasn’t as confident getting out of the house by herself because she wasn’t steady on her feet. Patricia’s GP explored this with her and mentioned that IPC Health’s Social Prescribing program may be able to connect her to local services and programs that could help with these feelings.
Once the referral was made, a Wellbeing Coordinator contacted Patricia and booked a time for a face-to-face conversation. Through a holistic assessment, the Wellbeing Coordinator and Patricia discussed that she had some physical pain due to arthritis which was stopping her from exercising. She acknowledged that she wanted to start moving more.
Patricia also mentioned that she loved to read but wasn’t a member of the local library. The books she read were from local opportunity shops. Because Patricia didn’t have much room for storage, she would have to return the books to a charity once read. The Wellbeing Coordinator talked about accessing the library as way to start making connections with people who shared her passion for books. The library was only a short distance from Patricia’s home and there was a book group run by a staff member. Patricia felt this would be a good fit for her.
Patricia agreed that attending her local senior hydrotherapy class, facilitated by an IPC Health physiotherapist, would help her arthritis. These activities were placed on her wellbeing plan as steps to increase her social connections and work towards building up her balance and physical strength to move about with more confidence.
The Wellbeing Coordinator followed up with Patricia who reported that she felt comfortable in the book group and would be returning. She also shared that the hydrotherapy session has assisted her movement and general confidence about being part of social groups again.
Patricia achieved the goals that she identified as part of her wellbeing plan. She has since joined the local library and visits regularly. Patricia has also increased other forms of physical movement thanks to the mobility and balance she’s gained through the hydrotherapy classes. The feelings of loneliness and isolation have improved and Patricia feels more connected to her community.
NEW REPORT
Community Health Centres and COVID-19: Impact and Experiences from the Pandemic
Canadian Association of Community Health Centres (July 2021)
Mobile COVID-19 response in Ottawa, Canada reaches vulnerable homebound clients
 South East Ottawa Community Health Centre’s (SEOCHC) Mobile COVID-19 Testing Team offers testing for high risk populations to mitigate the transmission of SARS-COV-2 and its impact on disproportionally affected, equity-seeking communities.
South East Ottawa Community Health Centre’s (SEOCHC) Mobile COVID-19 Testing Team offers testing for high risk populations to mitigate the transmission of SARS-COV-2 and its impact on disproportionally affected, equity-seeking communities.
In Fall 2020, the Centre quickly pivoted resources and stepped up to support city-wide pandemic response efforts with a small team of nurses and a nurse practitioner offering mobile COVID-19 testing five days a week. The team also participated in community outreach activities, going door-to-door to bring awareness of COVID-19 supports in high-risk neighborhoods. SEOCHC was supported by healthcare partners to receive training and setup the referral and test processing pathways. The team utilized its strengths in community health to offer testing and wrap-around community and social supports such as food, shelter, transportation, etc. The value of this service led to offering testing seven days a week and eventually taking on the responsibility for testing across the City of Ottawa.
Since October 2020, nearly 1800 mobile COVID-19 tests have been completed and SEOCHC’s nurses have travelled tens of thousands of kilometers across all corners of the region, including rural areas offering this service in the home. Monthly test positivity rates have consistently remained higher than Ottawa’s overall rates, reaching nearly 50% at the peak of the third wave. Over the last nine months, team members have witnessed the many barriers that high risk populations face in accessing testing such as financial barriers to accessing transportation or childcare or ability to take time off from work, mobility challenges, or mental health challenges which hinder access to testing. SEOCHC’s team has stepped up to support clients facing these and other complex barriers.
Stories from the past year really showcase the impact SEOCHC’s nurses have had on their clients:
- A young child refusing testing due to a previous negative experience had a pleasant experience being tested at home and was inspired by one of the CHC’s nurses to start wearing a mask.
- Multiple large families with children unable to travel have been thankful that the CHC’s nurses could come to the home and offer testing. One anxious child in a wheelchair, for instance, was comforted and encouraged by siblings while the nurse administered the test.
- Instances where parents were sick and unable to leave their children at home, were able to receive at home testing from SEOCHC’s nurses.
These experiences also enabled SEOCHC to identify gaps in care and to implement follow-up care, preventing these clients from falling through the cracks. This included referring symptomatic clients to a home monitoring program and offering symptom management to prevent hospitalizations.
SEOCHC’s testing team continues to accept referrals from public health, assessment/testing centres, congregate care settings, and other community health providers. The CHC’s target clients are those who have mobility challenges; have limited or no access to transportation; limited or no capacity to book appointments or attend testing centres; households with many young children or elderly; those living in hot spot neighborhoods; from newcomer, racialized, and/or low- socio-economic status populations.
The home visit is quick with a nurse in full PPE administering the test and assessing oxygen saturation at the door or entering the home for a short visit. All screening and assessments are completed virtually prior to the home visit to ensure staff have limited exposure to the virus and all follow-up is virtual unless there is a need for another home visit. The team includes nurses from a number of programs/services teams at the CHC each dedicating a portion of their work week to the mobile testing team while continuing to offer services to the centres other clients.
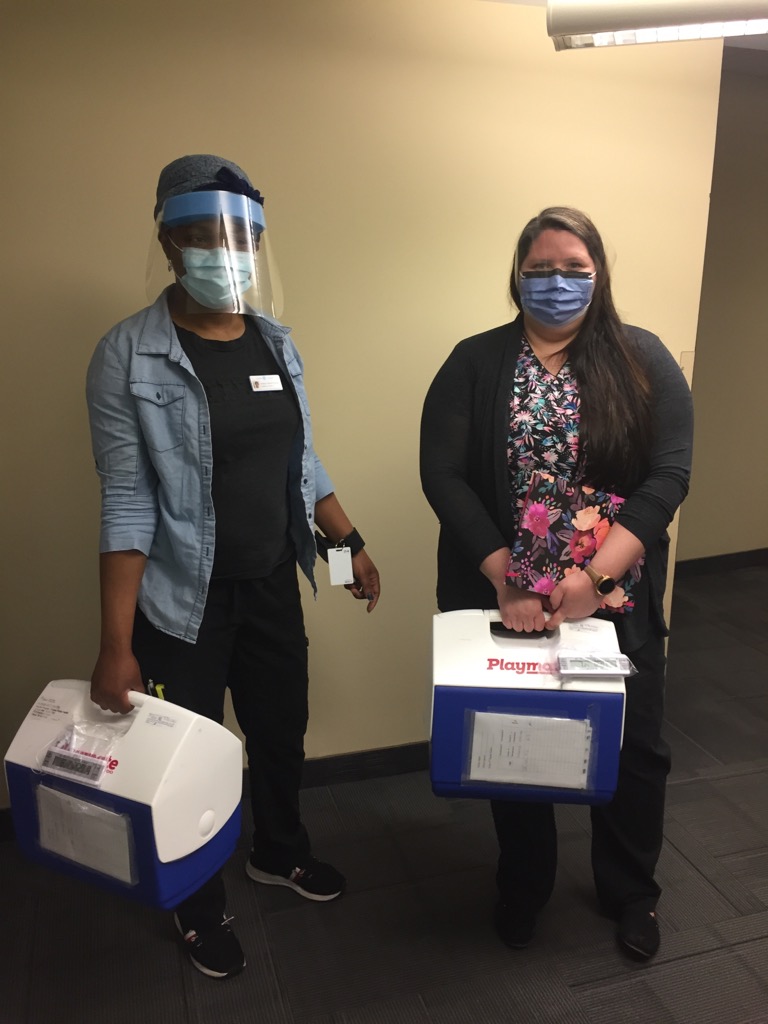
As vaccine supply became more readily available in March 2021, Ottawa area Community Health Centres were asked to step-up to support vaccinations for homebound individuals and families. In partnership with home care and the local public health unit, SEOCHC led the Ottawa’s network of CHCs in planning and executing homebound vaccinations across Ottawa for home care clients and clients of a regional program providing primary care outreach to seniors.
Ottawa’s CHCs faced and overcame many logistical challenges in order to administer vaccines to homebound groups. A secure process was developed to share client data across agencies. A custom mapping tool identified clusters of clients to create optimal travel routes and ensure vaccine viability while on the road. Dose allocation and planning across six CHCs was a complex endeavor due to staffing challenges and time constraints.
From March to August 2021, SEOCHC has dedicated 2-3 teams of nurses and community health workers each week for these vaccination efforts, with strong support from the CHC’s administrative team. In addition to completing its own list of clients, SEOCHC supported other CHCs and the local public health unit to take on additional clients as needed, and different strategies were used at the end of each day to ensure no available doses went unused within the allocated time period. The upfront administrative work of identifying clients on the mapping tool, calling and scheduling clients, and setting the daily travel routes for the teams has been resource-intensive but necessary for a smooth-running operation.
SEOCHC started offering homebound vaccinations in April 2021 and continue to offer first and second doses to clients across Ottawa. Thus far, the centre’s nurses have travelled tens of thousands of kilometers administering the COVID-19 vaccine to clients living in both urban and rural areas. In total, Ottawa’s six CHCs have administered vaccines to nearly 1800 homebound clients and their primary caregivers. Over 50% of those doses have been administered by the SEOCHC team.
CHC Inc’s Weitzman Institute: addressing the health and social needs of homeless youth
Exacerbated by the COVID-19 crisis, homelessness is a major public health challenge facing 4.2 million youth across the United States. It disproportionately impacts LGBTQ+ youth and youth of color. Nonetheless, early actions to intervene can help boost resilience and change the life trajectories of youth experiencing homelessness.
Community Health Centers often serve a vital role in actively addressing the health and health-related social needs of this population, including serving as the gatekeeper to vital social supports.
In early 2021, Community Health Center Inc‘s Weitzman Institute, based in Connecticut, USA, launched a youth-driven, action oriented research project to better understand the web of factors contributing to youth homelessness, and to identify evidence-based interventions that put a stop to youth homelessness in the U.S. and build healthier communities. The project receives generous support from the Aetna Foundation,
The team at the Weitzman Institute strives to transform the delivery of primary care through research, technology, education, and innovation. Examining and solving for the links between social determinants of health (e.g., housing insecurity) and health outcomes is central to this work.
Weitzman Institutes youth homelessness project centers its efforts in New Britain, Connecticut, given the significant health, education, and social disparities experiences in this community. The Institute established strategic partnerships with over 25 youth-serving entities in New Britain, including community-based organizations, local government, and the Consolidated School District of New Britain, to identify young people between the ages of 14 and 24 who have experienced homelessness.
In early 2021, project staff assembled a team of 15 young individuals as paid partners in research to examine the factors contributing to homelessness using an innovative community-based participatory research technique known as photovoice. Participants were trained in photography and provided cameras to capture visual representations of their everyday lives. Their pictures and stories bring their concerns to life, and urge community leaders and policymakers to take action.
Furthermore, the project team worked with its robust network of partners to examine barriers and facilitators to address the health and health-related social needs of youth experiencing homelessness. They conducted focus groups with youth-serving adults and completed 19 key informant interviews with stakeholders representing a myriad of community sectors and backgrounds.
The project is currently transitioning into its advocacy phase. The youth-led Photovoice Team is creating multimedia materials (e.g. podcasts, policy briefs, etc.) that inform policymakers, practitioners, and researchers on the factors that contribute to negative health outcomes facing youth experiencing homelessness. Project team members will be working with partners to create forums that strategically inform key leaders about findings and recommendations emerging from the research. They are also collaborating with the New Britain Herald on a special series spotlighting the stories of youth and the efforts of youth-serving adults.
Weitzman is proud of how the community has rallied behind this project, to elevate young voices and inspire youth-driven change across communities hurting from COVID-19 and homelessness. Given the success of this project, the team at the Institute strongly encourages other communities to tackle youth homelessness through similar research and advocacy initiatives.
Learning from the success of Victoria, Australia’s community health response to COVID-19
 Innovation, agility, clinical expertise and strong community connections – these were key elements of the successful community health response to COVID-19 in Victoria, Australia.
Innovation, agility, clinical expertise and strong community connections – these were key elements of the successful community health response to COVID-19 in Victoria, Australia.
A new report published by the Victorian Healthcare Association (VHA) — the state’s association representing Community Health Centres — details the vast array of service adaptations and innovations implemented by community health services (ie, CHCs) during 2020. These occurred as community health services supported and serviced their existing client groups, while expanding support to new population groups who were vulnerable to COVID-19 infection, social isolation, economic hardship and health risks.
Commissioned by the Victorian Department of Health, The community health response to the COVID-19 pandemic documents the introduction and acceleration of service and sector innovations during the pandemic in 2020 – many of which could offer sustainable benefits to Victoria’s healthcare system.
VHA CEO Tom Symondson said community health services were highly responsive and agile in their delivery of State and Federal government pandemic response programs including testing, social support, public health messaging and mental health programs.
“Widespread service innovation was achieved while community health services faced multiple challenges during the pandemic,” he said.
“Victoria’s community health services continued to deliver clinical and social support to their clients, while supporting – often leading – the wider public health effort to slow the spread of COVID-19 and reduce its social impacts. They did this while adapting to fast-changing government advice on restrictions and infection control and keeping their staff and clients safe from COVID-19 infection.”
Innovations and capabilities demonstrated by community health services during the pandemic included:
- the rapid transition to deliver services via telehealth
- supported isolation for people with COVID-19 and pathways to tertiary care, if required
- the translation of public health messages into multiple languages
- workforces that combined infection control and clinical expertise with social support skills
- the expansion of services beyond existing client groups to deliver support to people at risk of COVID-19 infection, other health issues, family violence and social isolation.
“Importantly, community health services were quick to identify the vulnerabilities and risks within their communities and responded with strategies that targeted and met the needs of Victoria’s diverse population groups,” Mr Symondson said.
Community health services are now looking to formalise and systematise the successes of the COVID-19 response, and to better integrate the sector’s capabilities into the wider Victorian healthcare system.





